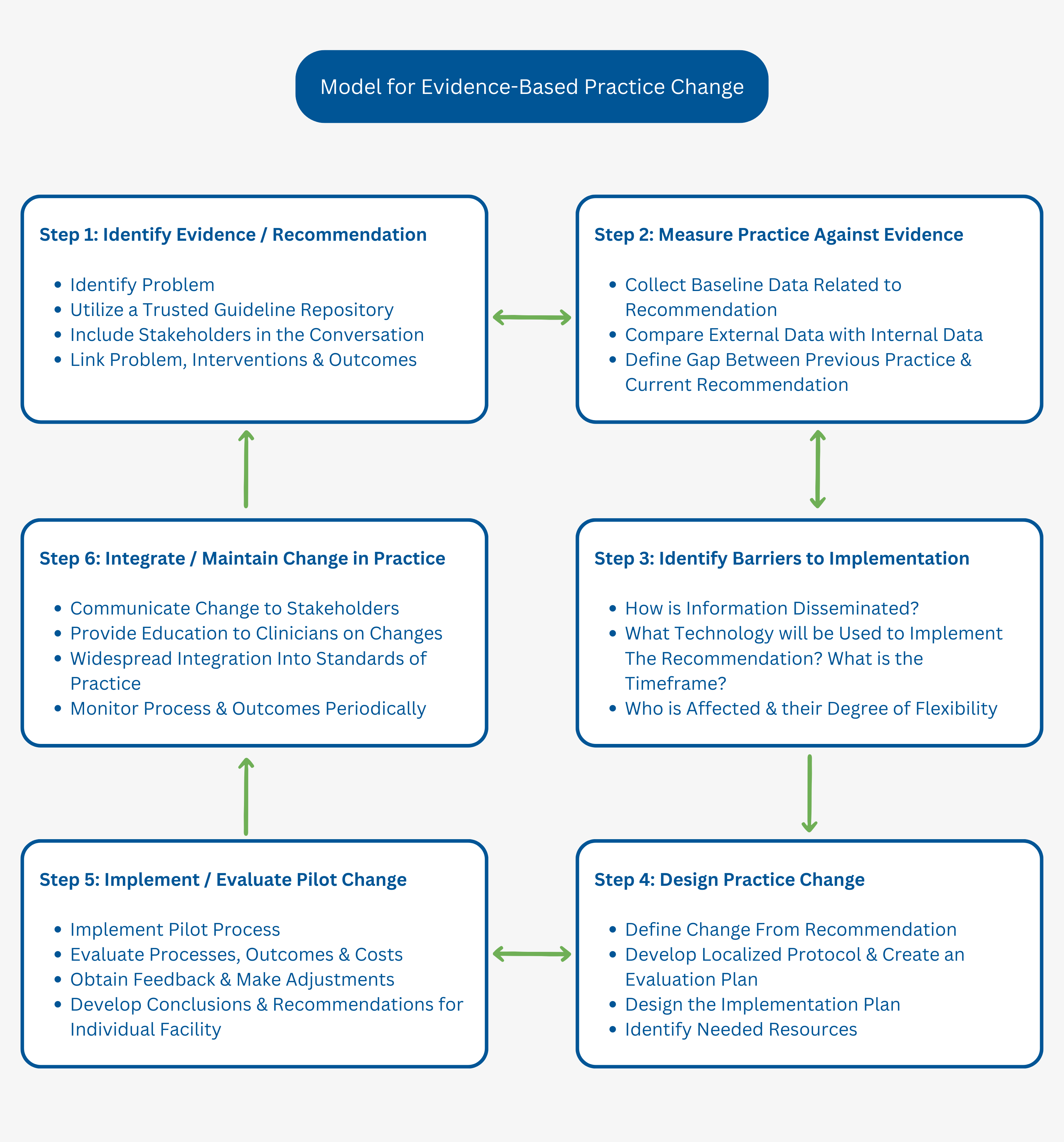
A while back, we kicked off a 7-step approach on how to implement guidelines or any specific guideline recommendations with an organization. We also looked closely at the first step of the process on how to identify some of these guideline as well as some factors to consider when determining guideline implementation priorities.
We have already assessed a need for change, and you have identified the recommendation you want to implement from Step 1 through utilization of a trusted resource; Guideline Central. Now what? In this article, we will be focusing on our second step – Measuring the state of your current practice, which will be broken down further into its own steps!
How you do that is through data collection. Collecting internal evidence and reviewing information relating to the recommendation is critical. Detailed information about the current state of clinical practice at a granular level provides insight into trends across populations and allows for comparisons in outcomes. One way to do that is through using implementation tools like this modified version of the Model for Evidence-Based Practice Change to reference as you start the process.
Process Steps To Consider When Analyzing & Measuring Data
- What is the current gap between the recommendation(s) you are attempting to implement and the current clinical practice at your organization?
- As an example, if you are considering adding a recommended medication to certain treatment plans, data on the current medication administration and outcome reports need to be reviewed.
- Adherence in terms of the percentage of occasions in which the care provided was consistent with the care recommended in guidelines should be one of the measures analyzed.
- What are the potential benefits for patients?
- In addition to clinical data, considering precedence, past practices, and internal metrics provide additional insights and connections not previously seen.
- Review data that provides information surrounding variations in care. For example, does care differ on the weekend? Do different patient populations have better responses to medications?
- Utilize internal data to ascertain how key metrics are performing to finding your organization’s baseline. This data can be related to a patient’s clinical state or outcome, medications, the setting of care encountered, or anything pertinent to patient care.
- Clean and analyze the data collected from your organization
- Data can be found in your electronic health record (EHR), patient surveys, or follow-up interviews depending on the recommendation you are implementing.
- Creation of a standardized data collection protocol now will be key to ensuring smooth transition during implementation.
Why all the data collection? A recommendation is only that; a recommendation. Know your data to know your organization, and your organization can fully integrate best practices seamlessly.
Future evidence-based quality improvement (EBQI) efforts will use this data after implementation to evaluate outcomes. Once your team is confident this recommendation is a fit for both your practice and your patients, you are ready for Step 3 to identify any potential barriers (and enablers) to implementing the recommendation that we will elaborate on in our upcoming posts.
Copyright © 2023 Guideline Central, All rights reserved.